Overview
The compounds in cannabis have promising potential for treatment of ALS, because of their ability to fight cell death and inflammation of the nervous system, elements in the disease process of ALS.
ALS (Amyotrophic Lateral Sclerosis) is a terminal neurodegenerative disease that damages motor neurons leading to progressive muscle wasting, weakness, and death.
Cannabis products have been shown to alleviate some common ALS symptoms, such as chronic pain, spasticity, lack of appetite and depression. Depending on the symptom you’d like to treat, the best marijuana strains for ALS would include either
THC, CBD, and limonene (for pain and spasticity). THC and CBG (for loss of appetite), or CBD, THC, CBG, BCP, limonene and linalool for depression.
Want to learn more about the research ? How cannabis works and how to choose marijuana strains for ALS? Read on.
➤ Apply for a medical marijuana card
Research on Marijuana and ALS
The cannabis plant contains at least 146 compounds called cannabinoids, most notably tetrahydrocannabinol (THC) and cannabidiol (CBD), as well as a host of other organic compounds such as terpenes and flavonoids.
THC directly bonds with the body’s two main cannabinoid receptors and has a neuroprotectant and anti-inflammatory effect. CBD doesn’t activate either receptor, but it blocks the enzyme (FAAH) that degrades anandamide. Commonly known as “the bliss molecule,” anandamide is a cannabinoid that plays a key role in maintaining the health of the ECS and can reduce anxiety and lower systemic inflammation, in addition to other benefits.
So researchers believe that compounds found within the cannabis plant may have therapeutic potential in the treatment of ALS. In one study, ALS mice were treated with THC before and after disease onset. Motor improvement was noted, and disease survival increased, which was thought to be due to a reduction in cell damage and death.
- A 2018 well-designed study using a pharmaceutical preparation of THC and CBD (Sativex/nabiximols)) for spasticity in ALS found that 55% of ALS patients reported overall improvements in spasticity and pain, compared with 13% in the placebo group. Furthermore, the drug was well tolerated with mild-moderate side effects including dizziness, lack of energy, and confusion.
- A 2004 study on ALS mice treated with THC before and after disease onset showed improvement in motor improvement and increased disease survival, believed to be linked to a reduction in cell damage and death.
- A 2005 study found that treating mice with the cannabinoid CBN could delay the onset of ALS-like symptoms.
Research on mice has found that modulating an ECS receptor on a daily basis delayed motor impairment and increased survival by 56%. In particular, raised levels of endocannabinoids were found in ALS mice models, as well as more CB2 receptors in the central nervous system, specifically in damaged or altered tissue.
CBD and ALS
CBD does not have the psychotropic effects of THC, and is thus often widely-available in jurisdictions where medical marijuana has not been legalized. A study performed on mice with ALS in 2010 found that small doses of CBD given to mice slowed down the progression of the disease.
A clinical trial currently underway in Australia is testing the effect of a CBD dominant oil on 30 subjects with ALS.
How Cannabis Works on ALS
The endocannabinoid system (ECS) exists in all vertebrates and helps regulate crucial functions such as sleep, pain, and appetite. The human body produces its own cannabinoids, which modulate and activate its various functions, but as its name suggests, the endocannabinoid system can also be modulated and activated by cannabinoids found in the cannabis plant.
A 2017 paper on cannabinoid pharmacology describes how the ECS has the ability to modulate the key traits contributing to neurodegenerative diseases such as ALS, and is “thus, emerging as a viable target for symptom alleviation or disease progression based on pharmacological modulation of endocannabinoid signaling.”
Studies on ALS animal models and ALS patients show some ECS dysregulation in the brain and spinal cord. However, this may well be a sign of the ECS doing its neuroprotective work rather than the dysregulation itself being a cause of the disease.
How to Use Marijuna for ALS
Although mostly based on preclinical studies, cannabis can potentially slow the progression of ALS, due to the antioxidative and neuromodulating properties of marijuana. It can also ease ALS symptoms such as pain, spasticity, loss of appetite, and depression.
Choosing the right marijuana strain for ALS can be challenging; there are thousands of chemovars out there and science is yet to clarify which is the best for ALS. The best bet for now is to narrow down your options by looking at the cannabinoids and terpenes that could help with ALS symptoms.
For pain and spasticity, the evidence suggests using the cannabinoids THC, CBD. The terpenes myrcene and limonene. BCP, linalool and humulene show potential for pain.
Cannabinoids THC and CBG can stimulate appetite , but there doesn’t seem to be much knowledge about which terpenes can enhance this effect.
And finally, for depression, CBD, THC, and CBG are believed to have antidepressant properties, along with the terpenes BCP, limonene, and linalool. Taking this into consideration, ACDC, Ringo’s Gift and Sour Tsunami strains could potentially help treat multiple sclerosis.
A word on dosing. Although each of our bodies interact with the compounds in cannabis differently, there is some clinical knowledge about general dosages. For patients with no/little prior experience with marijuana, 2.5mg THC is suggested as a starting dose. For those who can’t find relief with lower doses, 5mg THC is a moderate dose, and 10mg THC is suggested as an “experienced users only” dose.
Patients should wait 10-20 min between doses when taken by inhalation, 45min when taken sublingually, and 2 hours when ingested. It’s important to note that you can relieve symptoms even if you don’t get high, and that the recommended daily dose is no higher than 30mg THC. Higher doses are associated with increased chances of negative adverse effects, and very little additional therapeutic effect.
Please consult a medical practitioner experienced in cannabis treatment before making any treatment choices.
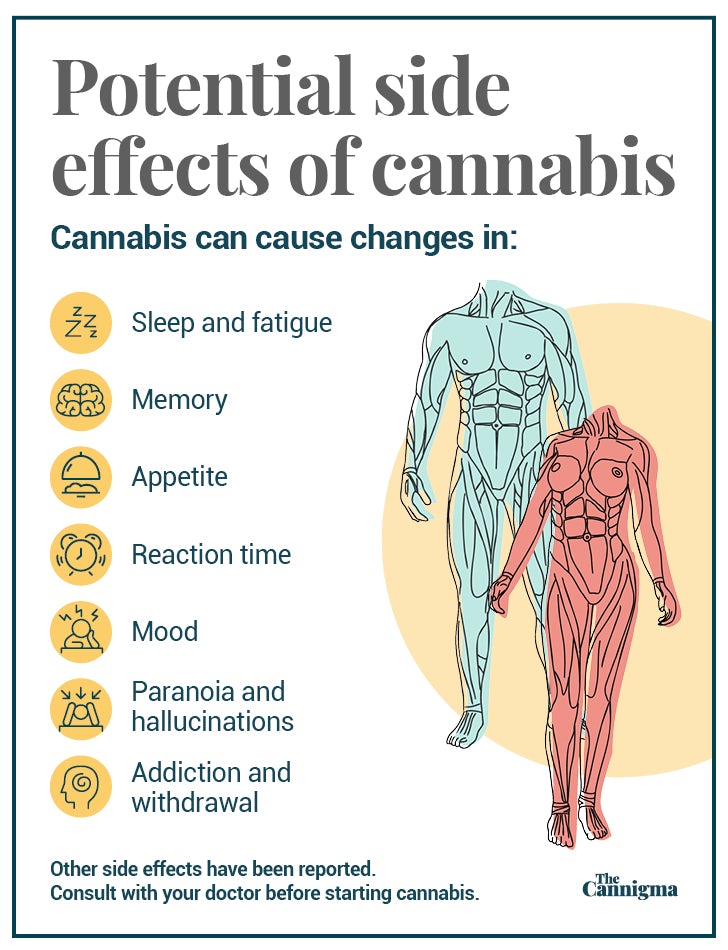
Potential side effects of cannabis use
Marijuana use can be habit forming and can make users more sluggish with decreased motor skills and reaction time when under the influence. Long-term effects can include cognitive impairment, a small risk of addiction, as well as an increased risk of developing a psychotic disorder. Further research is necessary to explore the potential interaction between other ALS medications and specific doses and forms of CBD and THC.
Alternative Treatments For ALS
Other than marijuana, there are additional alternative treatments for ALS or its symptoms, including traditional Chinese medicine, meditation, and dietary modifications.
Acupuncture
Although there are no clinical trials for the effectiveness of acupuncture in ALS, there are several case studies to support it, and it is a common treatment in Chinese medicine. There is one systematic review and meta analysis that is currently being conducted, aiming to “comprehensively verify the effects of acupuncture on ALS with evidence-based studies”.
Guided Meditation
Guided meditation can be used to help some of the common symptoms in ALS. One clinical study that investigated the effectiveness of an ALS specific meditation program found a significant difference between those who practiced meditation and those who didn’t. The study found that meditation improved a variety of symptoms, such as: quality of life, anxiety, depression, negative emotions and interaction with people and the environment.
Nutritional Support
People with ALS burn calories faster. This can easily lead to malnourishment, especially since people with ALS have trouble chewing and swallowing as the muscle weakness progresses. Nutritionists help caregivers and individuals to prepare frequent small meals that are high in calories, to prevent malnutrition, and to choose foods that are easy to swallow.
Sign up for bi-weekly updates, packed full of cannabis education, recipes, and tips. Your inbox will love it.

 Shop
Shop Support
Support