Marijuana and Multiple Sclerosis
Further studies are needed relating to MS and cannabis, but the studies published to date are encouraging and largely show that cannabis has a positive effect on MS. The fact that there is an approved medication (Sativex) available in some countries points to the efficacy of THC in treating MS-related muscle spasms, and calls for FDA approval are mounting. Given the few known side effects, cannabis may be a worthwhile supplementary treatment for patients with MS.
According to preliminary research, there are other cannabinoids and terpenes that show potential benefits for MS-related symptoms, such as CBN, myrcene, BCP and linalool (for insomnia), limonene and myrcene (for pain and spasticity), and BCP, humulene and linalool for pain only.
➤ Get your medical card now with The Cannigma Medical
Research on Medical Marijuana for MS
Over the last 20 years, various studies have delved into the relationship between cannabis and MS, with results leaning towards a positive relationship.
Although the widely cited CAMS study found no objective improvement on the Ashworth Scale of spasticity, it did find that patients receiving cannabis treatments had improved self-reports of spasticity and decreased pain. A follow up of this study found continued improvement after one year, suggesting that long-term treatment with cannabinoids may be of benefit, although the authors are careful to note that further study is required.
In a 2019 national study involving 427 MS patients who were using marijuana the majority (70%) of respondents reported that it helped with pain management, 56% said it helped sleep concerns such as insomnia, and 49% reported benefits for spasticity.
A 2012 study in the UK using THC capsules found significant improvement in muscle stiffness in MS patients, with twice as many patients in the treatment group showing improvement — as compared to the placebo group.
A UCSD study involving smoked cannabis found that it was superior to placebo in reducing spasticity in MS patients.
A meta-analysis of various studies relating to cannabis and MS found that a majority of patients (77%) report they use fewer opioids for pain when they supplement their treatment with cannabis. There was also a reduction in the use of anti-anxiety medication (72%) and sleep medications (67%). Overall, the authors of the analysis suggest cannabis supplementation may help reduce potentially addictive prescription medication use. This encouraging result could potentially help fight the opioid epidemic playing out in the USA and many other countries, leaving tens of thousands dead in the USA each year.
Although these studies are promising, and surveys of MS patients have shown that between 25% and 50% use cannabis as a treatment for their symptoms, more robust trials would certainly allow us to gain greater insight as to how marijuana can be utilized in the treatment of MS.
CBD and MS
Based on a large, double-blind clinical trial, the United Kingdom, Canada, and several European countries have approved nabiximols (Sativex®), a mouth spray containing THC and CBD in a 1:1 THC:CBD mixture. Sativex treats muscle control problems caused by MS, but it is not currently FDA-approved for use in the US.
CBD has been demonstrated to be well tolerated, both with continual use and in high doses of up to 1,500 mg a day, without significant impairment of psychological or bodily functions. However, a few studies linked CBD with some drug interactions and researchers note physician monitoring is warranted with elderly people, or with those with kidney and liver conditions.
How Cannabis Works on MS
The endocannabinoid system (ECS) exists in all vertebrates and helps regulate crucial functions such as sleep, pain, and appetite. The human body produces its own cannabinoids, which modulate and activate its various functions, but as its name suggests, the endocannabinoid system can also be modulated and activated by cannabinoids found in the cannabis plant. Because the entire system was only discovered in the past 30 years, scientists still have much to learn about the myriad ways cannabis affects the human body.
In a study involving both live mice and human blood samples, the researchers concluded that the ECS is out of balance in patients with MS, and there is evidence the ECS is activated in central nervous system attacks. There seems to be an anti-inflammatory effect of endocannabinoids (cannabinoids produced within the body), indicating either the body tries to protect itself from attacks to the neural sheath (a key component of MS) or that the body tries to mitigate the damage by releasing endocannabinoids. Further studies are needed to determine the exact role of the ECS in MS and the potential mechanism of protection, but this is a promising avenue in understanding the disease.
Using Marijuana for MS
There are a lot of marijuana varieties (AKA strains) out there, each with its own distinct chemical profile. But due to years of prohibition, health practitioners know very little about the best strains for MS, and patients are often left alone to do their own research until they find a match.
One thing that can help narrow down the possibilities, is learning about the different cannabinoids and terpenes that are suggested as a potential treatment for multiple sclerosis, and start the trial and error with chemovars that are rich in them. That being said, it’s important to note most of this knowledge is based on preliminary research, and you should always consult with a health practitioner with cannabis expertise.
For pain management and spasticity, both of the major cannabinoids THC and CBD show benefit, and the terpenes that can enhance these properties are limonene and myrcene. Terpenes that can help just with pain are BCP, humulene and linalool.
Chemovars for insomnia include these with THC and CBN, and terpenes such as myrcene, BCP and linalool.Taking this into consideration, ACDC, Ringo’s Gift and Sour Tsunami strains could potentially help treat multiple sclerosis.
When it comes to dosing marijuana, caution is needed as a lot of the common side effects of THC are dose dependent. Furthermore, THC has been known to show a biphasic effect where low doses cause one effect and high doses show the opposite. For instance, low doses can reduce anxiety while high doses can trigger anxiety.
The recommended doses for patients who are new to marijuana is 2.5mg THC, and 5mg for more experienced consumers. A maximum dose of 10mg should only be tried if lower doses aren’t effective.
The maximum daily dose shouldn’t exceed 30mg, as higher doses significantly increase the likelihood of adverse effects with very little effect on symptom improvement. In whole plant products, it should be noted that THC levels are often very high and average at around 15-25%. To take the example of a joint, a 1 gram joint would contain at least 150mg THC, the recommended amount for at least five days of treatment. For this reason, many patients look for balanced THC:CBD products with a lower THC concentration, use a tobacco substitute to dilute the flowers, or use other delivery methods such as tinctures and vapes.
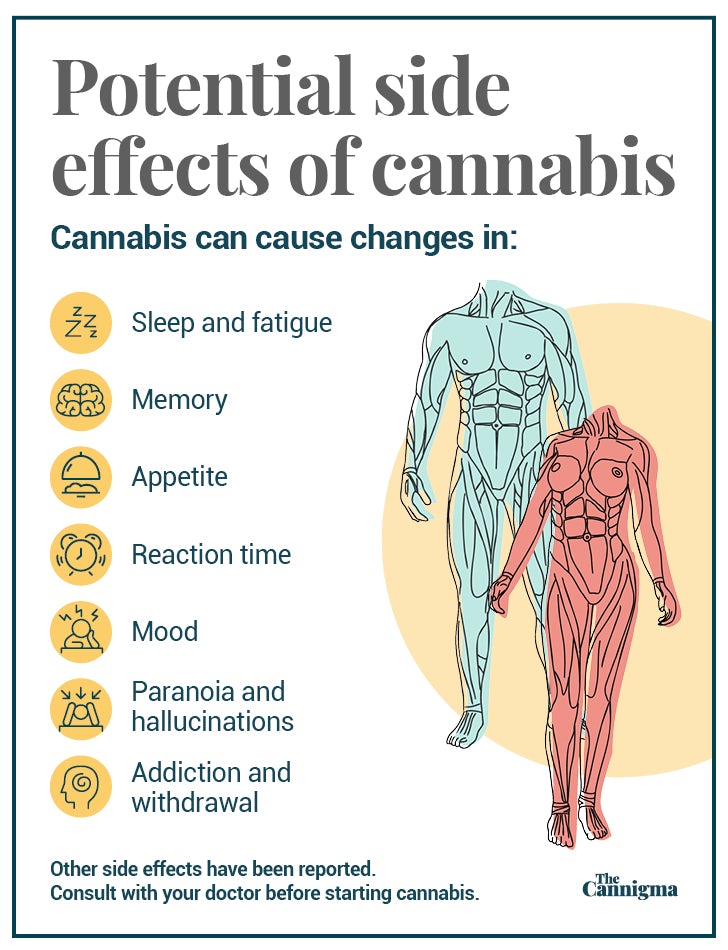
Potential side effects of cannabis use
Tiredness, confusion, and slowed motor control are known and common side effects of THC usage. Psychosis has also been known to be an adverse effect, though rare. It is worth noting that less than 5% of participants in any of the studies cited withdrew due to side effects. That being said, there are some strategies that can be adopted in order to mitigate some of these side effects, such as careful dosage and choosing the right cannabis variety.
THC seemingly has a low potential for addiction, with approximately 8.9% of long term users developing dependence. However, abrupt withdrawal from THC has been associated with cannabis withdrawal syndrome.
Alternative Treatments For MS
According to the National MS Society, diet, exercise, stress management and acupuncture can be effective complementary approaches for MS treatment.
Food and diet: MS specialists recommend a heart healthy diet, i.e. low fat high fiber — though there is no clinical evidence that a particular diet can cure or control MS. There is however some evidence for the benefits of foods such as omega 3 fatty acids, lipoic acid, ginkgo biloba, ginseng, green tea and vitamin D.
Exercise: A 2015 review of the literature suggests physical activity could potentially help spasticity, fatigue, mood, quality of life, cognition, and could even have neuroprotective effects. If you want to learn more about specific physical activities for MS, the authors of the study added a section with practical recommendations.
Stress management: One 2012 clinical study evaluated two groups, one that practiced relaxation breathing and progressive muscle relaxation twice daily, and another that didn’t. Researchers found that, “In patients in the intervention group, perceived stress and symptoms of depression were significantly decreased after 8 weeks of relaxation”. There are some practical guides for stress management in multiple sclerosis that could also help.
Acupuncture: A review of the literature on acupuncture and quality of life, fatigue, pain and spasticity in MS patients, found that “there is a striking paucity of literature available to describe its use or its efficacy… (but that) practitioners should not assume that acupuncture is not effective in this population but rather that the literature is insufficient to make claims either for or against its use.”
Sign up for bi-weekly updates, packed full of cannabis education, recipes, and tips. Your inbox will love it.

 Shop
Shop Support
Support