Marijuana for Migraines
People have been using cannabis to relieve migraine headaches throughout history. This remains a popular practice today as standard medications don’t always offer relief and come with significant side effects.
Recent medical research is beginning to provide evidence for the beneficial effects of cannabis and the involvement of the endocannabinoid system in migraines.
In fact, groundbreaking findings suggest that a deficient endocannabinoid system may be the underlying cause of migraines and some other difficult-to-treat conditions.
There are thousands of cannabis varieties out there, but research suggests that the best treatment for migraines would be with marijuana varieties that contain THC, CBD, beta-caryophyllene, and myrcene. However, many other cannabinoids and terpenes probably also play a role and future research will help to clarify these efficacy patterns.
What is the endocannabinoid system? How is it linked to migraines? Can marijuana offer relief? And if so, which cannabis products in particular? Here’s what the research says.
➤ Get your medical card now with The Cannigma Medical
Research on Medical Marijuana for Migraines
Despite the long history of cannabis use for migraines, there isn’t a lot of research in this area. However, the current findings are overwhelmingly positive and support the theory that endocannabinoid deficiency is one possible underlying cause of migraines.
One 2016 study by the University of Colorado examined the efficacy of medical cannabis in 121 people with migraines. The treatment was effective in 85.1% of the patients, reducing the number of migraines from an average of 10.4 to 4.6 headaches per month. It was noted that cannabis not only reduced the number of migraines but also aborted (stopped) them if taken when a migraine attack was happening.
Meanwhile, a 2019 study looked at the effects of medical cannabis in 316 patients with chronic migraines. In total, 88.3% of the patients reported improvement of migraines, with an average 42.1% reduction in monthly migraine frequency. Some patients experienced an even higher reduction (50% or more), and many reported improvements in sleep, anxiety, and mood.
Interestingly, the study also found that cannabis with a 20:1 ratio of THC to CBD resulted in better improvements than cannabis with a 1:1 ratio. This finding could be explained by the fact that unlike CBD, THC resembles anandamide in its function and effects.
Furthermore, a 2018 controlled animal study found that isolated THC reduced migraine pain in female rats, supporting the suggestion that cannabinoids may be useful in treating migraines in people.
Additionally, a 2001 review paper by the aforementioned Dr. Ethan Russo discussed historical records of successful cannabis use for migraines going back thousands of years. This review included particularly detailed case reports written by Western doctors between 1842 and 1942, when cannabis became a popular remedy for migraines. Dr. Russo concluded that “Based on the above review, it is convincingly the case that ‘medical marijuana’ deserves formal scientific scrutiny for migraine treatment.”
Also, there’s evidence that cannabis can help with the two main symptoms of migraines: pain and nausea. The pain-relieving effects of cannabis have been demonstrated by dozens of studies, so much so that the National Academies of Sciences, Engineering, and Medicine released the following statement in 2017: “There is conclusive or substantial evidence that cannabis or cannabinoids are effective for the treatment of chronic pain in adults.”
Meanwhile, the anti-nausea effects of cannabis are also backed by research, and cannabis-derived pharmaceutical drugs such as Marinol are already used to relieve specific types of nausea.
On the whole, while more high-quality studies are needed, the existing evidence demonstrates that medical cannabis can relieve migraines.
CBD for Migraines
Type III cannabis (CBD dominant) has been suggested as a potential treatment for migraines in a recent review of the literature. Since hemp based products (THC<0.3%) are often accessible over the counter, this option is often preferred by people that suffer from migraines.
According to the review “Chronic symptoms need around the clock treatment, including three times a day dosing. Dosing should start with 5–10 mg nightly during week 1, 5–10 mg twice a day during week 2, then 5–10 mg three times a day during week three, for a total of 30 mg. After a month, the dose may be increased to 20 mg three times a day, for a total of 60 mg. The maximum dose of CBD is patient- and illness-dependent; up to 600 mg/day has been well-tolerated in patients.”
However, make sure to choose CBD products from reputable brands and that has gone through third-party testing. If you are taking any prescription medications, make sure to check with your treating physician before you start any cannabis treatment.
How Cannabis Works on Migraines
The endocannabinoid system is an important biological system involved in maintaining a healthy state of balance in the body called homeostasis.
Consisting of cannabinoid receptors, endocannabinoids, and the enzymes that synthesize and break down endocannabinoids, this system helps regulate many critical processes, such as cognitive function, mood, metabolism, immunity, and pain.
So far, researchers have identified two cannabinoid receptors—CB1 and CB2. Although they are spread throughout the whole body, CB1 is particularly abundant in the central nervous system, whereas CB2 is commonly found in immune cells. These receptors are activated by two endocannabinoids made by the human body: anandamide and 2-AG.
Similarly, phytocannabinoids (plant-derived cannabinoids) such as THC and CBD are also able to interact with cannabinoid receptors.
Research studies indicate that the endocannabinoid system may interact with several processes involved in migraines.
One such process is the release of the brain chemical serotonin by platelets, small cell fragments found in the blood. Studies suggest that endocannabinoids can prevent this release and that individuals with chronic migraines have reduced levels of anandamide and 2-AG in their platelets.
More importantly, endocannabinoids have been linked to a part of the brain called the trigeminovascular system, which is widely considered to play a central role in causing migraine attacks. Research suggests that endocannabinoids regulate this system through the CB1 receptor.For example, one 2004 study found that anandamide inhibits trigeminal neurons, suggesting a mechanism for how endocannabinoids can prevent migraines.
More importantly, a follow-up 2011 study reported that administering anandamide to rats with migraine-like headaches reduced both neuron activation in the trigeminovascular system and the associated pain.
Similar findings were reported by a 2015 study of the FAAH enzyme, which is responsible for breaking down anandamide. The researchers almost completely relieved migraine-like pain in mice when they deleted this enzyme or administered compounds that prevented it from working.
Findings such as these led researchers to suggest that a dysfunctional endocannabinoid system may even be responsible for migraines.
This idea was first proposed by Dr. Ethan B. Russo, the Director of Research and Development for the International Cannabis and Cannabinoids Institute (ICCI) and one of the leading medical cannabis experts, when he unveiled his theory of clinical endocannabinoid deficiency (CED) in 2001.
According to this theory, insufficient endocannabinoid levels might be the cause of a wide variety of difficult-to-treat conditions, including inflammatory bowel syndrome, fibromyalgia, and migraines.
The strongest evidence for this hypothesis came from a 2007 study which found that individuals with chronic migraines had lower levels of anandamide in their cerebrospinal fluid than healthy people. The study’s researchers proposed that these insufficient levels can result in the failure of the endocannabinoid system to inhibit the trigeminovascular activation that produces migraines.
Lastly, there’s evidence that certain genetic variations of the CB1 receptor can predispose a person to migraines, which further supports the CED theory because anandamide works primarily through this receptor.
Using Marijuana for Migraines
There are thousands of cannabis varieties out there, each with a unique chemical profile that contains not only different amounts of THC and CBD, but also other “minor” cannabinoids and also different terpenes. This makes finding the best marijauna strain for migraine a potentially challenging endeavour. But with the help of the current scientific literature, you can at least narrow down your possibilities.
As we can see from the medical research on cannabis and migraines, THC (rather than CBD) has more evidence as a migraine treatment. And when it comes to terpenes, in his rich review on marijuana for migraines, Russo suggested BCP and pinene as potential terpenes that could alleviate migraines thanks to their anti-inflammatory properties.
And indeed, in a more recent study, migraine patients testified that the chemovar “OG Shark” was their preferred choice. This THC dominant chemovar is characterized as BCP dominant, with myrcene as the secondary terpene.
So it seems scientifically speaking, if you’re trying to choose a marijuana strain for migraines, the evidence supports the use of high THC/ low CBD with BCP (or pinene) as the prime terpene, and myrcene as the secondary one.
A word about dosing. People tend to believe more is better, but in the case of cannabis often the opposite is true. There is a dose dependent relationship between efficacy and side effects (AKA the biphasic effect), primarily based on THC content. Of course we are all different, but as a general rule, 2.5mg of THC is the threshold dose, 5mg is a moderate dose and 10mg is a high dose.
The general recommendation is anywhere between 15-30 mg THC daily, with the lower the effective dose the better to limit tolerance, dependency, and side effectsץ More than that and the risk of side effects spikes, and there’s no evidence going over this dose is effective. If you’re having trouble estimating 30mg THC, imagine a joint that weighs 1 gram, from a chemovar that has 10% THC. this would mean there’s 100mg in the entire joint. So 30mg would be just a little bit more than a third of this joint.
Note that a lot of the scientific knowledge we have about cannabis components such as cannabinoids and terpenes is based on preclinical research – ie not on human subjects. Though they are mostly defined as GRAS (Generally Recognised As Safe), you should consult your cannabis physician before choosing your treatment.
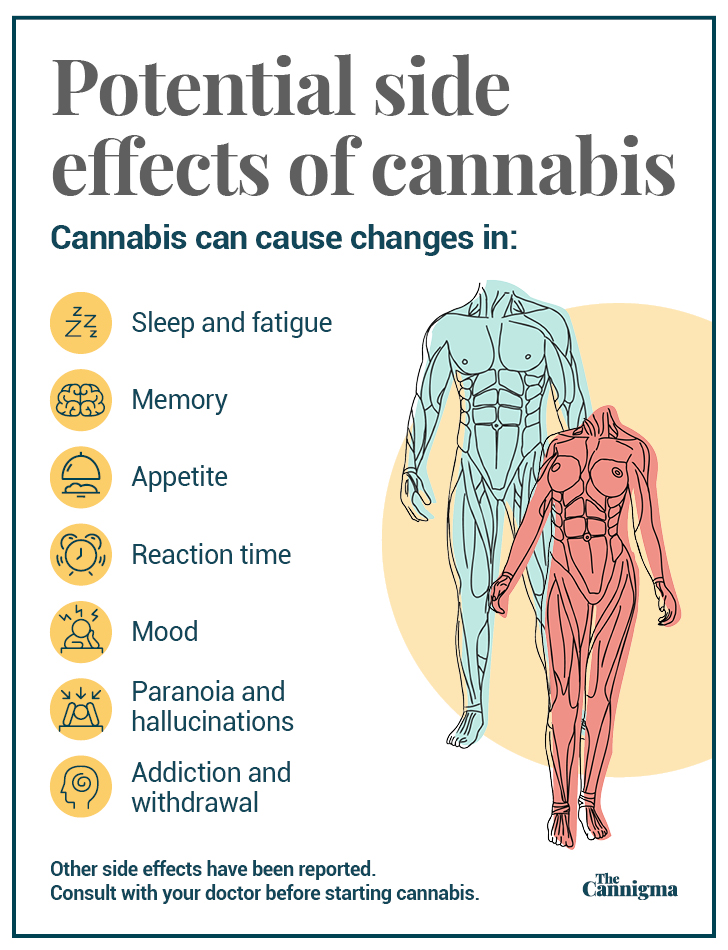
Potential side effects of cannabis use
Although cannabis appears to be an excellent option for treating migraines, it does have some unwanted effects.
In particular, the major barrier to increased medical use of cannabis is its psychoactive side effects, which include euphoria, memory impairment, and anxiety. In addition, cannabis can cause other side effects such as dry mouth, drowsiness, and fatigue.
Ultimately, however, cannabis is considered a safe substance. This is especially the case when we compare it to pharmaceutical drugs used to treat migraines, such as NSAIDs. A related benefit of cannabis is that it helps people reduce the use of opioids, which are sometimes prescribed for chronic migraines despite their addictive properties and ability to induce medication overuse headache (MOH).
Sign up for bi-weekly updates, packed full of cannabis education, recipes, and tips. Your inbox will love it.

 Shop
Shop Support
Support