Overview
Cannabis has been used to relieve inflammation and autoimmune disorders throughout history. What’s more, research shows that the body’s endocannabinoid system regulates immune function and may play a role in the rise and suppression of autoimmune disorders, including lupus.
This interaction provides a plausible explanation for why some lupus sufferers find relief with cannabis. What’s the connection between the endocannabinoid system and lupus? Can cannabis be a natural alternative or supplement to pharmaceutical drugs? Here’s what you need to know.
The Endocannabinoid System
Consisting of endocannabinoids, their receptors, and the enzymes that synthesize and break them down, the endocannabinoid system (ECS) helps our bodies maintain a healthy state of balance called homeostasis. Only discovered in the 1990s, this system plays a major role in human health, regulating immune function, mood, cognition, pain, sleep, metabolism, and other key processes.
The major components of the endocannabinoid system are the endocannabinoids anandamide and 2-AG, which are produced inside the body as needed. These compounds act through two cannabinoid receptors: CB1 and CB2. Whereas CB1 is abundant in the central nervous system, CB2 is chiefly found in immune cells, highlighting its role in regulating immune system function and inflammation.
These receptors also interact with phytocannabinoids (plant-derived cannabinoids) such as CBD and THC, which explains how cannabis can affect processes in the body.
The endocannabinoid system plays a key role in regulating immune function and by extension inflammation.
Most notably, endocannabinoids have been shown to affect the growth and survival of immune cells, the production of proinflammatory cytokines, the activation of immune cells, and the migration of inflammatory cells. Together, these effects are particularly useful for reducing the excessive immune system activation and inflammation that characterizes autoimmune disorders.
Indeed, recent research investigations show that the endocannabinoid system is involved in disorders characterized by autoimmunity and inflammation, such as multiple sclerosis, celiac disease, and rheumatoid arthritis.
For example, one study found that people with multiple sclerosis had higher levels of anandamide in their brains compared to healthy subjects. Similarly, a 2008 study of arthritis patients reported that they had elevated levels of anandamide and 2-AG in the synovial fluid of their joints.
Finally, a 2013 study in people with celiac disease reported that they had higher levels of CB1 and CB2 receptors in parts of the digestive tract affected by the condition and that these levels returned to normal after the disease went into remission.
Research looking specifically at the endocannabinoid system in lupus patients is scarce. This is in good part due to the fact that research in cannabis has been hindered to its legal status around the world.
The only major study in this area compared the levels of endocannabinoids in healthy individuals and those with lupus, highlighting two key findings:
- People with lupus had elevated levels of 2-AG, which is the main endocannabinoid that binds to CB2 receptors
- There was a link between higher 2-AG levels and lower disease activity, suggesting that the endocannabinoid system was effectively suppressing the lupus
The researchers of this study concluded that “our data confirm that the eCB system critically modulates inflammatory responses and auto-immunity and support evidence of cannabis-based medicine as immune-modulating agents.”
Current data indicates that this system plays a major role in controlling inflammation and immunity and that targeting it through cannabis-based drugs is a promising treatment for autoimmune disorders like lupus.
More studies on the involvement of the endocannabinoid system in lupus are needed. Especially since treatment in Lupus has not been very successful until the present time.
Cannabis & Lupus
There is little research looking at the medical use of cannabis in lupus patients. Indeed, there’s currently only one active clinical trial in this area; it looks at the effects of JBT-101 (lenabasum), a synthetic cannabinoid drug, in people with lupus.
This study will attempt to see if this cannabis-based medicine can relieve lupus pain and inflammation by calming the overactive immune responses that cause the disease. JBT-101 has already shown positive results in studies of other inflammatory and immune-related disorders, including cystic fibrosis and systemic sclerosis.
There is much more evidence that cannabis can relieve the key symptoms of lupus, namely inflammation and pain.
The anti-inflammatory benefits of THC, CBD, and other cannabis-based preparations have been demonstrated in animal models and some human studies of those with autoimmune disorders, such as multiple sclerosis, rheumatoid arthritis, colitis, and hepatitis.
For example, a 2006 study found that the cannabis-based drug Sativex reduced pain caused by rheumatoid arthritis (RA). This study is particularly relevant because both lupus and RA are characterized by joint pain and inflammation that’s caused by an overactive immune system.
Similarly, the pain-relieving effects of cannabis have been reported in dozens of human studies. Most notably, a 2015 systematic review of 28 clinical trials of cannabinoid use for chronic pain concluded that “There was moderate-quality evidence to support the use of cannabinoids for the treatment of chronic pain.” This evidence is strong enough that chronic pain is the most common qualifying condition for medical cannabis.
In addition, there’s research evidence that cannabis can relieve other issues that can occur in lupus, such as headaches, seizures, and nausea.
Lastly, there are anecdotal reports of lupus patients who found relief by using cannabis. While these aren’t rigorously conducted clinical trials, it does offer hope to Lupus sufferers who are suffering from disabling pain in their joints and other parts of their body.
To summarize, more studies are needed to investigate whether cannabis can alleviate lupus. However, there’s plenty of evidence that cannabis can relieve pain and inflammation, including cases where the underlying cause is autoimmunity.
Side Effects
The major side effects of cannabis are psychoactive and include memory impairment, anxiety, euphoria, and paranoia.
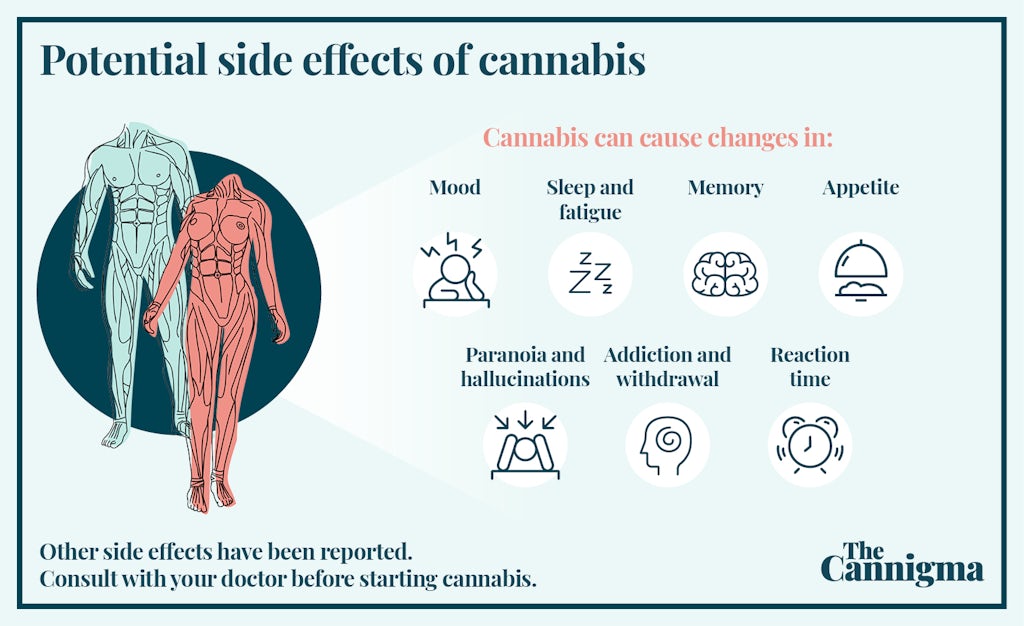
These side effects are one of the main reasons why many people turn to preparations rich in CBD, the non-psychoactive cannabinoid. While all types of cannabis can cause minor side effects such as sleepiness, tiredness, dry mouth, and changes in appetite, some do more than others. However, cannabis is a generally safe substance that’s been used for thousands of years, and its side effects compare favorably with many pharmaceutical drugs used to treat lupus, such as NSAIDs, corticosteroids, and immunosuppressive medications. And they are certainly a more attractive alternative for chronic pain than widely prescribed opiates which have caused an epidemic in many areas.
Conclusion
Research looking at the link between lupus and the endocannabinoid system is just beginning, and it’s too early to say anything conclusive.
Nonetheless, we know that the ECS is involved in healthy immune function and that targeting it through cannabis-based preparations can offer relief for the inflammation and pain that characterize lupus.
Additionally, research shows that cannabis can help with other symptoms of lupus as well, such as headaches, seizures, and nausea.
While this evidence by itself isn’t strong enough for clinicians to recommend cannabis for lupus, it does offer patients an alternative form of treatment, especially when standard medications aren’t working or are causing serious side effects.
Potential side effects of cannabis use

Sign up for bi-weekly updates, packed full of cannabis education, recipes, and tips. Your inbox will love it.

 Shop
Shop Support
Support